Interview to MD PhD Claudio Liguori
Sleep and Epilepsy Centers, Neurology Unit, Department of Systems Medicine – University of Rome Tor Vergata, UNIROMA2
This month will be held the Think Tank about Neurodegeneration and Sleep. Which are your expectations?
I am glad and honored to be part of the workshop participants at the 5th Neurodegeneration and Sleep Think Tank. I expect to hear some of the leading experts on relevant topics such as major neurodegenerative diseases and sleep disorders, how these two factors are related. I am curious to be updated on the latest research developments in this field. The also called World Sleep Forum 2021 will be divided between key public lectures and five workshops. In the last ones, we will have the opportunity to discuss the most salient arguments in small groups. I am very excited to participate and bring my inputs.
In the Think Tank, it will be many discussions about neurodegeneration and biomarkers useful for early detection. Could you give us a definition of biomarkers of neurodegeneration? Why is crucial their early identification?
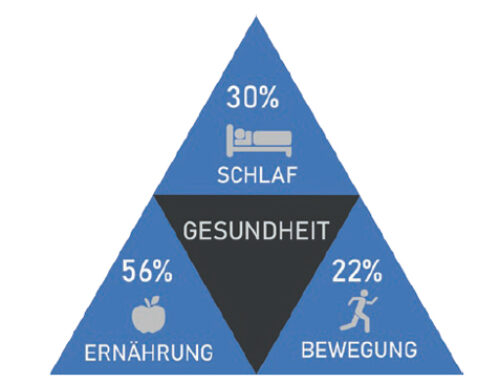
Biomarkers of neurodegeneration can be defined as the signs/symptoms that validate the neurodegenerative process, also in the very early stages of the disease. Initially, diagnoses of neurodegenerative disorders were achieved after the patients’ death. Now we can find in vivo biomarkers through neurological/cognitive examinations, biofluids or neuroimaging, etc. to diagnose the neurodegenerative disorders and start as soon as possible the proper treatment and follow-up. Early identification of biomarkers is critically important to implement treatments (also neuroprotective ones) against the neurodegenerative mechanism. The earlier the treatment is applied, the more significant is the outcome. Even for therapeutic purposes, an adaptation of lifestyle, an adjustment of diet, a greater attention to habits of daily life can have a neuroprotective effect if implemented in time.
Based on your research related to this topic, what are your main findings?
Concerning Alzheimer’s disease, we identified the alteration of the sleep-wake cycle very early compared with the cognitive disorders. In addition, we found a parallelism between the disturbance in nighttime sleep and both the cognitive disorders and cerebrospinal-fluid biomarkers of Alzheimer’s disease pathology (beta-amyloid and tau proteins). Moreover, we observed how sleep-disordered breathing go to alter Alzheimer’s disease biomarkers. This proves the argument that if we improve sleep or treat sleep disorders, we can protect against the neurodegeneration process.
Why are sleep and sleep-wake rhythms crucial for studying neurodegenerative diseases?
Sleep represents about a third of our life, in which a considerable number of phenomena take place. Some of these events are proven to be right neuroprotective phenomena. Sleep is a dynamic process that has effects on physical and cognitive functions. By ensuring a regular sleep-wake cycle, the organism can only reap benefits.
It is necessary to perform longitudinal studies and monitoring patients for many years to understand their neurodegeneration. In some cases, the follow-up can be up to 15 years. To avoid such long trials, what kind of studies do you think can be done?
By the time the pathology occurs, the neurodegenerative process in the brain has already been initiated. Grading patients according to the severity of the biomarkers found can be an option. For example, for patients with REM sleep behavior disorder (RBD), brain scintigraphy to monitor the dopaminergic system is performed. From this, we can see the degenerative process early and start a neuroprotective treatment. The result of this exam can be integrated with validated methods that simultaneously consider many clinical symptoms, such as depression, insomnia, excessive daytime sleepiness, hyposmia, in patients with RBD. In case all these symptoms co-occur, the risk of developing alpha-synucleinopathies is very high and a pre-determined follow-up with regular/frequent visits should be planned.
In the last years, there is a frequent discussion about how engineering and medicine can cooperate for new and promising results. What are your thoughts in this regard?
As a clinician, there is initial skepticism. The neurologist wants to see the patient with her/his own eyes. Despite this, the 60-minute clinical visit is not enough to get a complete clinical picture of the patient. And this is where we think the help of technology is relevant. Having devices that can provide us with data on the patient’s daily routine, amount of sleep and light exposure is of great importance. Validated algorithms that provide long-term patient data can be a powerful tool.
Do you think new technologies are capable of monitoring biomarkers?
Many technologies are widely used and can give insights about motor activity, blood oxygenation, etc. There is an extreme need to validate these algorithms. Having a score obtained from a validated algorithm can be easier to be accepted universally than the score provided by a single clinical observation.
Do you think new technologies can find new biomarkers?
Much research needs to be done to find additional biomarkers (or to incorporate them in a single instrument) through new technologies. The use of new approaches, data analysis, and increasingly sophisticated algorithms could probably lead to the identification of biomarkers of neurodegeneration.
How do you see the future of neurodegeneration research?
Much more attention to elements outside the neurodegenerative process per se. An openness in looking at factors outside the body, such as sleep rather than the proteins. In addition, I expect an approach given by the integration of different specialists, in the sense that the patient can be visited by different specialists, sleep experts, cognitive experts, and experts in neuroimaging, for example.
Over the years, you have won many awards, including one presented during The Fire Within international symposium. Do you have any advice for young researchers for a successful career?
Be curious as much as possible and try to understand the phenomena you study. Do not accept the events that occur but ask questions and seek answers. That was how the publication on orexin in Alzheimer’s was successful [1]. Also, you have to be passionate. In physiology, it is studied that the brain learns when it is motivated. It is essential to have the freedom to follow intuition. To do this it is crucial to read, update and confront. Certainly, events such as the Think Tank help the scientific community in updating, confronting and networking.
[1] Liguori C. Orexin and Alzheimer’s Disease. Curr Top Behav Neurosci. 2017; 33:305-322.
doi: 10.1007/7854_2016_50. PMID: 28012089.

Interviewer
Oriella Gnarra, PhD student, Sleep-Wake-Epilepsy Center | NeuroTec, Department of Neurology, Inselspital, Bern