
Sleep-disordered breathing as a multidisciplinary disease: The pulmonologist’s point of view
Oana Claudia Deleanu, MD, PhD, Lecturer at University of Medicine and Pharmacy, Bucharest, Romania
Sleep-related breathing disorders (SRBDs) are characterized by abnormal respiration during sleep and include a wide spectrum of disorders, e.g. obstructive sleep apnea (OSA), central sleep apnea (CSA), sleep-related hypoventilation, sleep-related hypoxemia disorder etc. [1]. The knowledge of normal sleep physiology is essential for understanding SRBDs pathophysiology. Normal sleep is composed of two major phases, NREM (non-rapid eye-movement) sleep and REM (rapid eye movements) sleep. NREM is the predominant one and is characterized by cardiovascular balance due to higher parasympathetic tone which controls the homeostasis and leads to the reduction in heart rate and blood pressure. REM sleep is characterized by eye movement, muscle twitches and skeletal muscle atonia. It is constituted of tonic and phasic stages. Unlike NREM phase, REM is dominated by cardiovascular instability. Heart rate and blood pressure vary a lot during REM sleep depending on switching parasympathetic or symphatetic control [2].
Central sleep apnea occurs more frequently during REM sleep than NREM sleep that may result from the increasing ventilation during REM [3]. Obstructive sleep apnea (OSA) occurs more frequently during NREM sleep [2].
Central sleep apnea (CSA)
CSA is defined by recurrent suspensions of breathing during sleep with no associated ventilatory efforts. CSA is believed to result from the failure of the ventilatory drive, but the etiology is unknown. CSA likely occurs in patients with underlying central neurological disorders, whereas OSA is found in patients with obesity. However, CSA and OSA are related to each other. There is evidence that central events determine instability of the breathing pattern and that this instability may provoke obstructive events [4].
Sleep-related hypoventilation
Hypoventilation entails an inadequate alveolar ventilation for maintaining normal gas exchange, resulting in hypoxaemia and hypercapnia. Obesity represents the most common cause for hypoventilation and the combination of obesity and hypoventilation is referred to as the obesity hypoventilation syndrome. Obese patients demonstrate an increased demand for ventilation, a slight respiratory muscle weakness and diminished respiratory compliance [4].
Obstructive sleep apnea (OSA)
OSA is a common disorder with increasing prevalence due to the obesity epidemic and greater public and physicians’ awareness [1]. About three decades ago, its prevalence was estimated as 4 % for men and 2 % for women [5]. However, the recent studies show OSA can be found in almost half of male population, which will probably lead to changes in the definition of the disease [6].
Obstructive sleep apnea involves a significant reduction or even cessation of airflow during sleep which can be defined as episodes of upper airway failure. These episodes are frequently associated with oxyhemoglobin desaturation and awakenings from sleep [7].
The syptomatology is insiduous which leads to a long-lasting course before the patient is guided for an evaluation. As a result, about 92 % and 80% cases are undiagnosed in women and men, respectively. The nocturnal and diurnal symptomathology varies, however, the diurnal sleepiness is the most debilitating symptom, reducing the quality of life [7].
OSA should be diagnosed and treated promptly. Currently, the treatment strategy is mostly guided by the severity of the disease assessed by the apnea-hypopnea index (AHI). Subjects with mild apnea (AHI = 5-14.9/h) can be offered a variety of options, while for the patients with moderate (AHI = 15-30/h) to severe apnea (AHI > 30/h) continuous positive airway pressure (CPAP) remains the first-line treatment. From less invasive towards the most invasive, treatments can be resumed as following:
- General measures and behaviours such as weight loss, alcohol avoiding 4-6h before sleep are elements of the conservatory treatment
- Oral appliance
- CPAP
- BiPAP
- If the non-invasive treatment fails, surgical options should be offered
- Combination approaches can be also considered [8].
Recently, the Baveno classification based on the analysis of the European Sleep Apnoea Database cohort (ESADA) Registry was proposed to characterize OSA and to guide therapeutic strategy. In this study the patients were statified based on symptoms and comorbidities according to Baveno classification system, and sex-related differences have minor significance. The groups with severe symptoms and less comorbidities vs. those with milder symptoms and moe comorbidities have similar hypoxemia load. Moreover, symptoms rather than comorbidities should be considered stronger indications for treatment. In each group stratified by Baveno classification, at least 70 % patients needed positive airway pressure (PAP) therapy based on clinical decision guided by AHI. After 24-36 months of treatment, according to Baverno classification, group A (minor symptoms and comorbidities) did not show any result of the treatment. With treatment, group with minor comorbidities and severe symptoms, group with minor symptoms and severe comorbidities and group with both severe symptoms and comorbidities were associated with improvement in either or both parameters. Therefore, the AHI index is essential for the diagnosis, but Baverno classification provides a better stratification of OSA patients which can contribute to a more appropriate management strategy [9]. The further search of other important variables associated with organ risks and prognosis is ongoing, which is also a part of the large-scale international project Sleep Revolution.
Overlap syndrom
COPD and OSA frequently co-exist, being defined as an overlap syndrome. Patients with overlap syndrome are exposed to even higher cardiovascular risks and higher risk of unfavourable outcomes. The main problem in overlap syndrome is severe hypoxemia, especially nocturnal hypoxemia. The need for the right and timely diagnosis and identification of both pathologies is obvious. The treatment options and the outcomes are different, as these patients being in high-need of oxygen and CPAP [10].
Why it is important to treat?
OSA is very important because it is often associated with coronary artery disease, hypertension, cardiovascular pathology, depression and other diseases [11]. In 2012, the analysis of a cohort of 77000 patients demonstrated that OSA is associated with all-cause mortality in patients under 50 years [12]. A group with mild or CPAP-treated OSA had similar cardiovascular risks compared to the population without OSA while a group with severe, untreated OSA showed high cardiovascular mortality risk [13].
Due to daytime sleepiness and low vigilance OSA patients are at high risk for driving accidents which defines social significance of the disease. Screening strategies aimd at identification of subjects at high risk for driving accidents are being investifated in order to improve safety on the road. Commercial drivers show a high prevalence of OSA and due to the obesity epidemy, the incidence of OSA-related car accidents is increasing [14, 15].
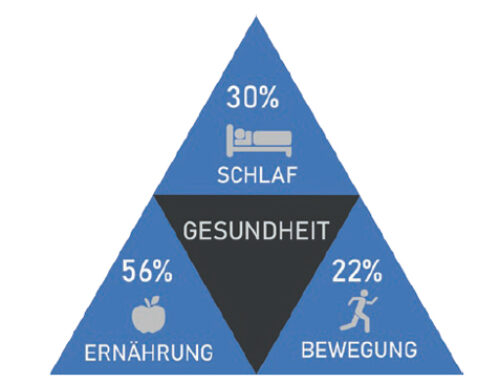
Due to the association with various pathologies and risks, a multidisciplinary team is crucial for the management of a patient with OSA. SDB was first demonstrated in the 1960s. Since then, SDB became a known widely prevalent risk factor for numerous medical and socio-economic problems. OSA leads to sleep disruption and fragmentation, which have deleterious effects as sleep is an important, although often neglected, component of every person’s health and well-being.
References
- Burman D. Sleep Disorders: Sleep-Related Breathing Disorders. FP Essent. 2017;460:11-21.
- American College of Chest Physicians Sleep Medicine Syllabus. 2008, p. 82.
- Lovering AT, Fraigne JJ, Dunin-Barkowski WL et al. Hypocapnia decreases the amount of rapid eye movement sleep in cats. SLEEP. 2003;26(8):961-967. doi.org/10.1093/sleep/26.8.961
- Randerath W, Verbraecken J, Andreas S et al. Definition, discrimination, diagnosis and treatment of central breathing disturbances during sleep. Eur Resp J. 2017;49:1600959; DOI: 10.1183/13993003.00959-2016
- Goetting C, Downey III R. Sick, symptomatic and undiagnosed. 2010.
- Heinzer R, Vat S, Marques-Vidal et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310-318. DOI: https://doi.org/10.1016/S2213-2600(15)00043-0
- Wickramasinghe H. Obstructive Sleep Apnea,Updated. 2020.
- Morgenthaler TI, Kapen S, Lee-Chiong T et al. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29(8):1031-5.
- Randerath W, Herkenrath S, Treml Met al. Evaluation of a multicomponent grading system for obstructive sleep apnoea: the Baveno classification. ERJ Open Research 2021 7: 00928-2020; DOI: 10.1183/23120541.00928-2020
- Owens RL, Malhotra A. Sleep-Disordered Breathing and COPD: The Overlap Syndrome, Respir Care. 2010;55(10):1333–1346.
- Leung RS, Bradley TD. Sleep apnea and cardiovascular disease. Am J Respir Crit Care Med. 2001 Dec 15. 164(12):2147-65.
- Rich J, Raviv A, Raviv N, Brietzke SE. All-cause mortality and obstructive sleep apnea severity revisited.Otolaryngol Head Neck Surg. 2012; 147(3):583-7.
- Young T, Finn L, Peppard PE et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008; 31(8):1071-8.
- Bonsignore M. Sleep apnea and its role in transportation safety. F1000Res. 2017;6:2168.
- Bonsignore M, Randerath W, Schiza S et al. European Respiratory Society Statement on sleep apnoea, sleepiness and driving risk. Eur Respir J. 2020 [In press]. DOI:10.1183/13993003.01272-2020